The arrival of a newborn is a joyous occasion, but for mothers who have undergone a cesarean section, the postpartum period can be accompanied by unique challenges. Recovery from major surgery, adjusting to motherhood, and managing pain and discomfort all contribute to a complex experience. Understanding the specific needs of mothers after a cesarean is crucial to ensure a smooth transition and optimal well-being.
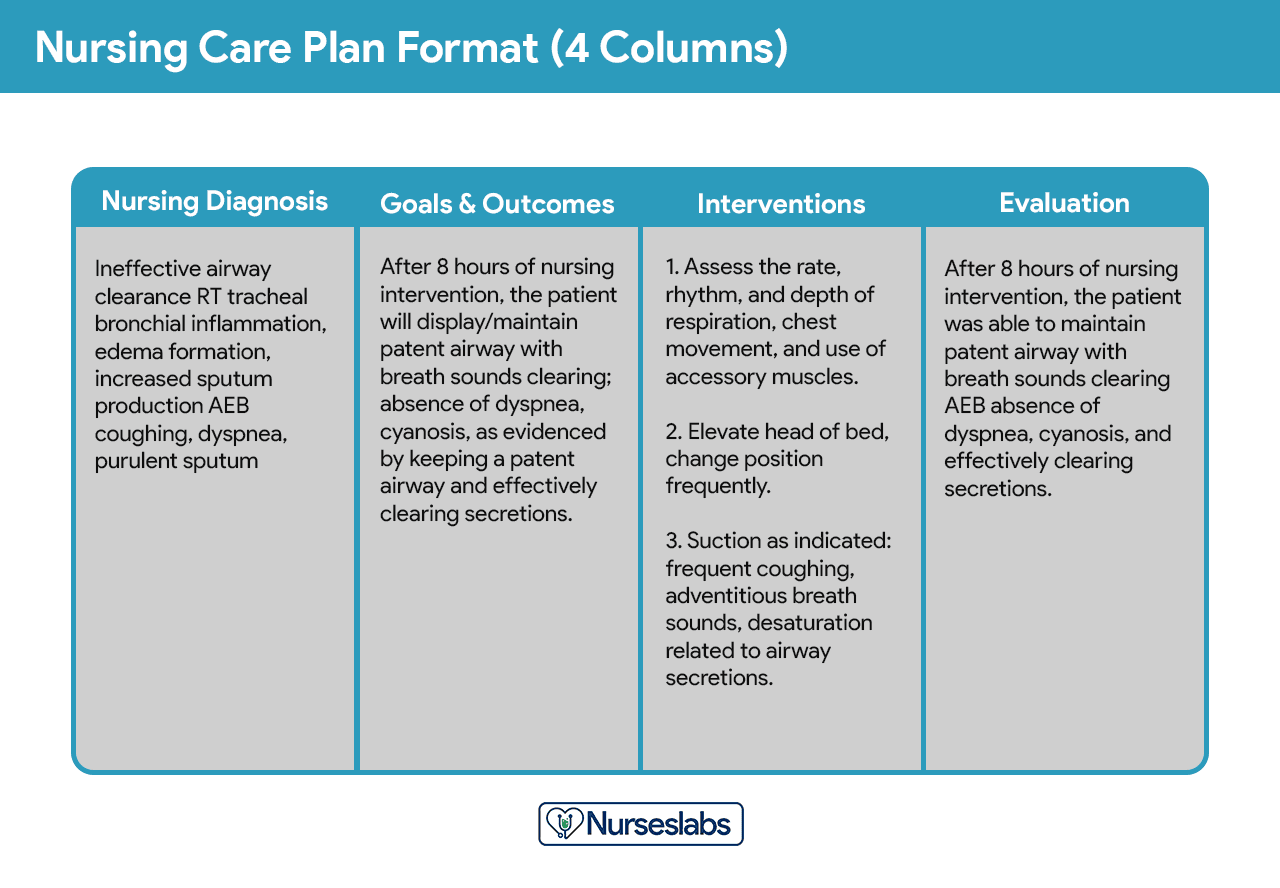
Image: sarseh.com
A comprehensive nursing care plan plays a vital role in guiding the postpartum recovery process for cesarean mothers. This plan considers the physical and emotional aspects of their needs, ensuring they receive the necessary support and interventions to heal and thrive. From pain management to wound care, breastfeeding challenges, and emotional support, this guide explores the essential elements of postpartum cesarean care.
Understanding Postpartum Cesarean Care
Postpartum care following a cesarean section focuses on addressing the immediate needs of the mother and her newborn. While the primary focus is on surgical recovery, it also encompasses emotional support, pain management, breastfeeding assistance, and education to empower mothers in their postpartum journey.
The care plan is tailored to the individual mother’s needs, considering factors like her medical history, the type of cesarean performed, and her overall health. It’s a collaborative effort involving nurses, doctors, and other healthcare professionals to ensure a safe and comfortable recovery.
Key Components of Postpartum Cesarean Care
A holistic postpartum cesarean care plan encompasses various aspects, including:
- Pain Management: Cesarean sections involve incision and surgery, resulting in pain that requires careful management. This may include medications like pain relievers, epidural analgesia, or nerve blocks.
- Wound Care: The surgical incision requires meticulous care to prevent infection and promote healing. This involves regular wound cleansing, monitoring for signs of infection, and providing instructions for home care.
- Physical Recovery and Mobility: Post-cesarean recovery involves promoting mobility and strength to minimize the risk of complications like blood clots or pneumonia. This can include early ambulation, breathing exercises, and leg exercises.
- Breastfeeding Support: While a cesarean birth doesn’t directly impact breastfeeding, some women may face challenges due to pain, fatigue, or positioning. This can include latch assistance, pumping support, and education about breastfeeding techniques.
- Emotional Support and Counseling: The postpartum period can be emotionally challenging for any mother, but particularly for those who have undergone surgery. Providing emotional support, counseling, and resources for coping with postpartum mood disorders is essential.
- Nutrition and Hydration: Proper nutrition and hydration are crucial for recovery. Nurses will provide guidance on dietary needs, ensuring adequate calorie intake and fluids to support healing.
- Education and Discharge Planning: Providing mothers with education about wound care, pain management, and other aspects of postpartum recovery empowers them to manage their care at home. Discharge planning ensures they have the necessary resources and support for a smooth transition.
Postpartum Cesarean Care: A Closer Look

Image: www.coursehero.com
Pain Management
Pain management is a central aspect of postpartum cesarean care. The goal is to provide effective pain relief while minimizing side effects and allowing for early mobility. The most common methods include:
- Medications: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, are often prescribed for mild to moderate pain. Stronger medications, like opioids, may be necessary for more intense pain.
- Epidural Analgesia: An epidural catheter, typically used during labor, can be left in place after delivery to provide continuous pain relief. This method allows for frequent pain relief and early mobilization.
- Nerve Blocks: A single injection of local anesthetic into specific nerves near the incision site can provide pain relief for several hours.
Nurses closely monitor mothers for pain levels, adjusting medications and treatment strategies as needed. It’s crucial for mothers to communicate their pain levels honestly to ensure effective pain management.
Wound Care
Wound care after a cesarean section is essential for preventing infection and promoting healing. Nursing care includes:
- Cleaning and Dressing: The incision is frequently cleaned with sterile solutions, and a gauze dressing is applied to protect the wound from contamination.
- Monitoring for Infection: Nurses closely monitor the wound for signs of infection, such as redness, swelling, warmth, drainage, or foul odor. Any concerns should be immediately reported to the doctor.
- Education: Nurses educate mothers about wound care at home, including proper cleaning, dressing changes, and signs of infection to watch for.
Mothers should follow these instructions carefully to ensure proper wound healing and minimize the risk of complications.
Physical Recovery and Mobility
Early ambulation after a cesarean is encouraged to prevent complications like blood clots (deep vein thrombosis), pneumonia, and constipation. With proper support, mothers can start to walk within a day or two of surgery. Nurses can help with:
- Assisted Ambulation: Nurses can help mothers walk and provide support with a walker or crutches in the initial days.
- Leg Exercises: Nurses will teach mothers simple leg exercises to improve circulation and prevent blood clots. These exercises can be done in bed or while sitting.
- Breathing Exercises: Deep breathing and coughing exercises help to expand the lungs and prevent pneumonia. Nurses will demonstrate these exercises and encourage mothers to practice them regularly.
As mothers progress, they can gradually increase their activity levels, starting with short walks and gradually increasing the distance and intensity as they become stronger.
Current Trends in Postpartum Cesarean Care
The field of postpartum cesarean care is continually evolving, with ongoing research and evidence-based practices shaping the best approaches. Some current trends include:
- Emphasis on Early Mobilization: Research is increasingly demonstrating the benefits of early ambulation for postpartum cesarean recovery. Minimizing bed rest and encouraging early movement helps reduce the risk of complications and promotes faster recovery.
- Non-Pharmacological Pain Management: There’s growing interest in exploring non-pharmacological pain management options like heat therapy, massage, and aromatherapy to reduce the reliance on medications and minimize side effects.
- Personalized Care: The focus is shifting towards individualized care plans that consider the mother’s unique needs and preferences. This includes providing options and allowing mothers to actively participate in their recovery decisions.
- Support for Breastfeeding: Efforts to support breastfeeding after cesarean have increased, recognizing the importance of breastfeeding for both the mother and baby’s health. This includes providing comprehensive breastfeeding education, latch assistance, and access to lactation consultants.
- Addressing Mental Health: Recognizing the potential for postpartum mood disorders after cesarean, there’s a focus on early screening and providing access to mental health resources and support.
Tips and Expert Advice
Here are some tips for mothers recovering from a cesarean section:
- Communicate Your Pain: Don’t hesitate to inform your nurses or doctor about your pain levels, even if it seems minor. Effective pain management is crucial for your recovery.
- Follow Wound Care Instructions: Adhere strictly to the wound care instructions you receive. This includes keeping the wound clean and dry, changing dressings as directed, and monitoring for any signs of infection.
- Move Regularly: It may seem daunting at first, but even small movements like walking around your room can make a big difference in your recovery. Engage in physical activity as tolerated by your body.
- Seek Support: Don’t be afraid to ask for help from your partner, family, or friends. They can provide emotional support, assistance with household tasks, and help with caring for your baby.
- Address Mental Health: Postpartum mood disorders are common, so be mindful of your emotional well-being. Don’t hesitate to reach out to a mental health professional if you’re struggling.
- Attend Follow-Up Appointments: Be sure to attend all scheduled follow-up appointments with your doctor to monitor your recovery and address any concerns.
Remember that recovery takes time. Be patient with yourself and focus on taking small steps toward regaining your strength and well-being. If you have any questions or concerns, don’t hesitate to ask your healthcare team. They are there to support you through each step of your recovery.
FAQs
1. What are the common complications after a cesarean section?
Common complications after a cesarean section include infection, bleeding, blood clots (deep vein thrombosis), wound dehiscence (separation of the wound), and uterine infection (endometritis). Pain management can also be a challenge and may lead to opioid dependence.
2. How long does it take to recover from a cesarean section?
Recovery from a cesarean section can vary depending on the individual, but most women experience significant improvement within a few weeks. Full recovery, including returning to normal activity levels, can take several months. However, every individual’s recovery is unique, so it’s important to listen to your body and avoid overexertion.
3. Can I have a vaginal delivery after a cesarean section?
Yes, it’s possible to have a vaginal delivery after a cesarean, known as a vaginal birth after cesarean (VBAC). However, this is not always possible and requires careful consideration and evaluation by your healthcare team. Factors like the reason for the previous cesarean, the type of incision, and the mother’s overall health are taken into account.
4. How can I prepare for a cesarean section?
Preparation for a cesarean section involves discussing the procedure with your doctor, gathering information about recovery, and organizing support for your postpartum period. It’s also helpful to plan for childcare, meal preparation, and other practical needs during your recovery. Discussing your concerns and preferences with your doctor beforehand is essential.
Nursing Care Plan For Postpartum Cesarean Section
https://youtube.com/watch?v=gEsCIfZ7oho
Conclusion
A comprehensive nursing care plan is essential for supporting mothers recovering from a cesarean section. From pain management and wound care to promoting physical recovery, emotional support, and breastfeeding assistance, the plan encompasses various aspects of their needs. With the latest trends emphasizing early mobilization, personalized care, and support for mental health, the field of postpartum cesarean care continues to evolve, offering greater comfort and well-being for mothers.
Are you interested in learning more about postpartum cesarean care, or do you have any questions about this topic? We’d love to hear from you and provide further information.





