Imagine a man struggling to urinate, experiencing frequent and urgent trips to the bathroom, and feeling like his bladder never completely empties. This is a common scenario for men suffering from benign prostatic hyperplasia (BPH), a condition that affects the prostate gland and leads to urinary problems. As a nurse, understanding these problems and developing a nursing diagnosis is crucial for providing effective and compassionate care.
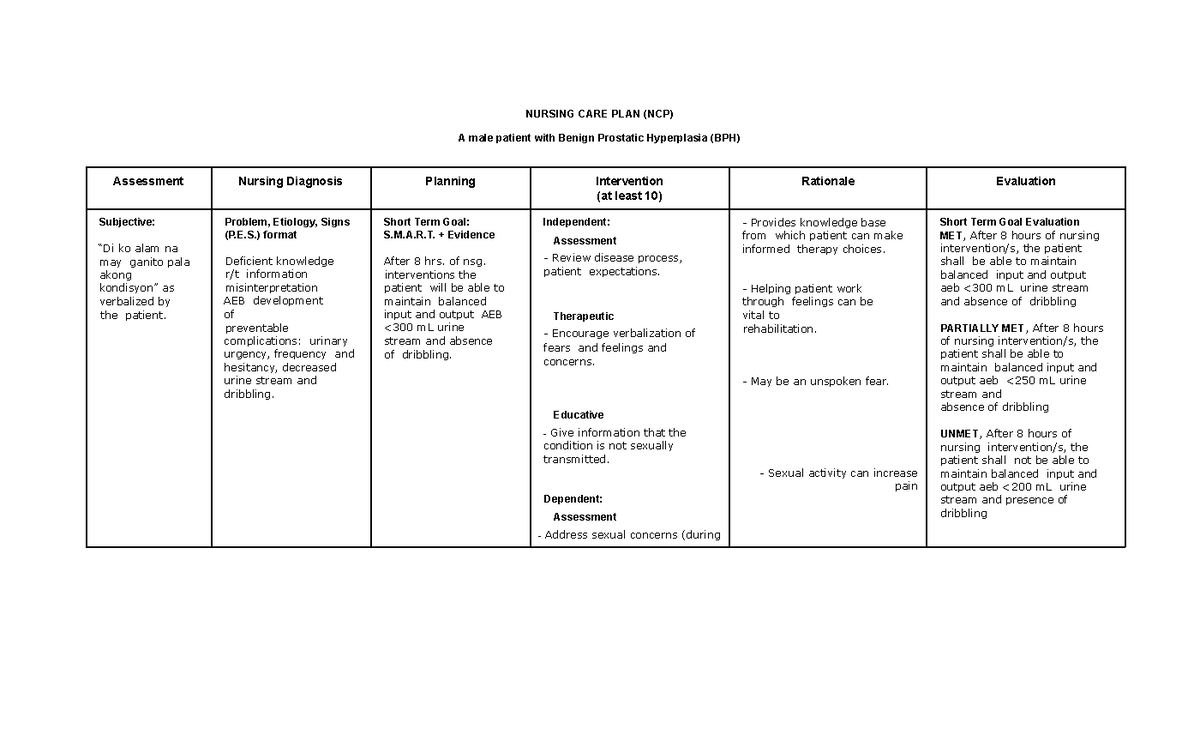
Image: lunfardo.com.ar
Benign prostatic hyperplasia (BPH), also known as prostate gland enlargement, is a common condition affecting men as they age. The prostate, a small gland located below the bladder, starts to grow abnormally, putting pressure on the urethra, the tube that carries urine out of the body. This pressure can lead to a range of urinary symptoms, affecting a man’s quality of life significantly. Nursing diagnosis provides a framework for recognizing and addressing the specific needs of patients with BPH, leading to better health outcomes.
Understanding the Basics of Benign Prostatic Hyperplasia
What is Benign Prostatic Hyperplasia?
BPH is a non-cancerous enlargement of the prostate gland. It occurs due to the growth of prostate cells, which increase with age. The prostate surrounds the urethra, the tube that carries urine from the bladder. This enlargement compresses the urethra, making it difficult for urine to flow out of the bladder.
Who is at Risk for BPH?
While BPH is a common condition, some men are more prone to developing it. Risk factors include:
- Age: BPH is more common in older men, with the majority of men experiencing some degree of prostate enlargement by the age of 80.
- Family History: Men with a family history of BPH are more likely to develop the condition.
- Race: African American men have a higher risk of developing BPH and experiencing more severe symptoms.
- Lifestyle Factors: A diet high in saturated fat and a lack of exercise can increase the risk of BPH.

Image: www.studypool.com
Nursing Diagnosis for Benign Prostatic Hyperplasia
Nursing diagnoses provide a framework for understanding and addressing the individual needs of patients. For patients with BPH, the primary focus is on managing urinary symptoms and improving quality of life. Some common nursing diagnoses for BPH are:
1. Impaired Urinary Elimination
This nursing diagnosis is applicable when a patient experiences difficulty voiding, an inability to control urination, or a change in the amount or frequency of urine. Symptoms of urinary elimination problems associated with BPH include:
- Hesitancy: Difficulty starting urination.
- Weak Stream: Urine flow is slow and weak.
- Dribbling: Urine leaks after urination.
- Frequency: Urinating more often, especially at night.
- Urgency: Sudden, strong need to urinate.
- Nocturia: Waking up at night to urinate.
2. Urinary Retention
This nursing diagnosis is used when a patient is unable to completely empty their bladder. Urinary retention can lead to discomfort, infections, and even kidney damage. Signs of urinary retention include:
- Feeling like the bladder is not completely empty after urination.
- Straining to urinate.
- Increased frequency, especially at night.
- Pain or discomfort during urination.
3. Acute Pain
Patients with BPH can experience pain related to urinary retention, infection, or other complications. Pain can be felt in the lower abdomen, pelvis, or back, and can be sharp, throbbing, or aching. This nursing diagnosis allows nurses to address the patient’s pain and provide comfort.
4. Constipation
BPH treatments, such as medications, may cause constipation as a side effect. This is particularly important to consider when evaluating patients for urinary dysfunction.
Nursing Interventions for BPH
Once a nursing diagnosis has been established, nurses can implement interventions to:
- Promote Urinary Elimination: Provide a private, comfortable bathroom environment, encourage fluid intake, and assist with voiding techniques.
- Manage Pain: Administer prescribed pain medications, assess pain level regularly, and teach relaxation techniques.
- Prevent Complications: Monitor for signs of urinary retention, infection, and other complications. Implement measures to prevent these risks, such as frequent bladder emptying and promoting good hygiene.
- Educate the Patient: Provide information about BPH, treatment options, and self-care strategies. This includes teaching the patient about medication management, bladder control techniques, and lifestyle modifications.
- Promote Regular Bowel Movements: Encourage patients to maintain a regular exercise routine and a diet rich in fiber. In cases of constipation, administer stool softeners or laxatives as prescribed.
Collaborative Care for BPH
Nurses play a crucial role in managing BPH by working closely with other healthcare providers, including physicians and urologists. This collaborative approach ensures comprehensive care for patients and helps address the various aspects of BPH management.
Collaborative care with physicians may include:
- Monitoring vital signs, urinary output, and other relevant parameters.
- Administering medications, including alpha-blockers, 5-alpha reductase inhibitors, and other drugs that help relieve symptoms and manage the condition.
- Assisting with surgical procedures when necessary, including transurethral resection of the prostate (TURP) or minimally invasive treatments.
Collaboration with other healthcare professionals may include:
- Working with physical therapists to develop bladder control exercises and improve pelvic floor muscle strength.
- Collaborating with dieticians to discuss dietary modifications and proper hydration techniques.
- Providing counseling and support to patients and their families to address concerns and provide emotional support.
Nursing Diagnosis For Benign Prostatic Hypertrophy
Conclusion
Nursing diagnosis is a critical tool for nurses managing patients with benign prostatic hyperplasia. By recognizing the potential for impaired urinary elimination, urinary retention, acute pain, and other complications, nurses can develop individualized plans of care to improve patients’ quality of life and prevent worsening symptoms. Understanding the risk factors, treatment options, and collaborative care strategies allows nurses to play a vital role in the comprehensive management of BPH. Remember, patience, compassion, and effective communication are essential for providing quality care to patients with BPH.





